Benign Blood Disorders
Our Treatment Philosophy
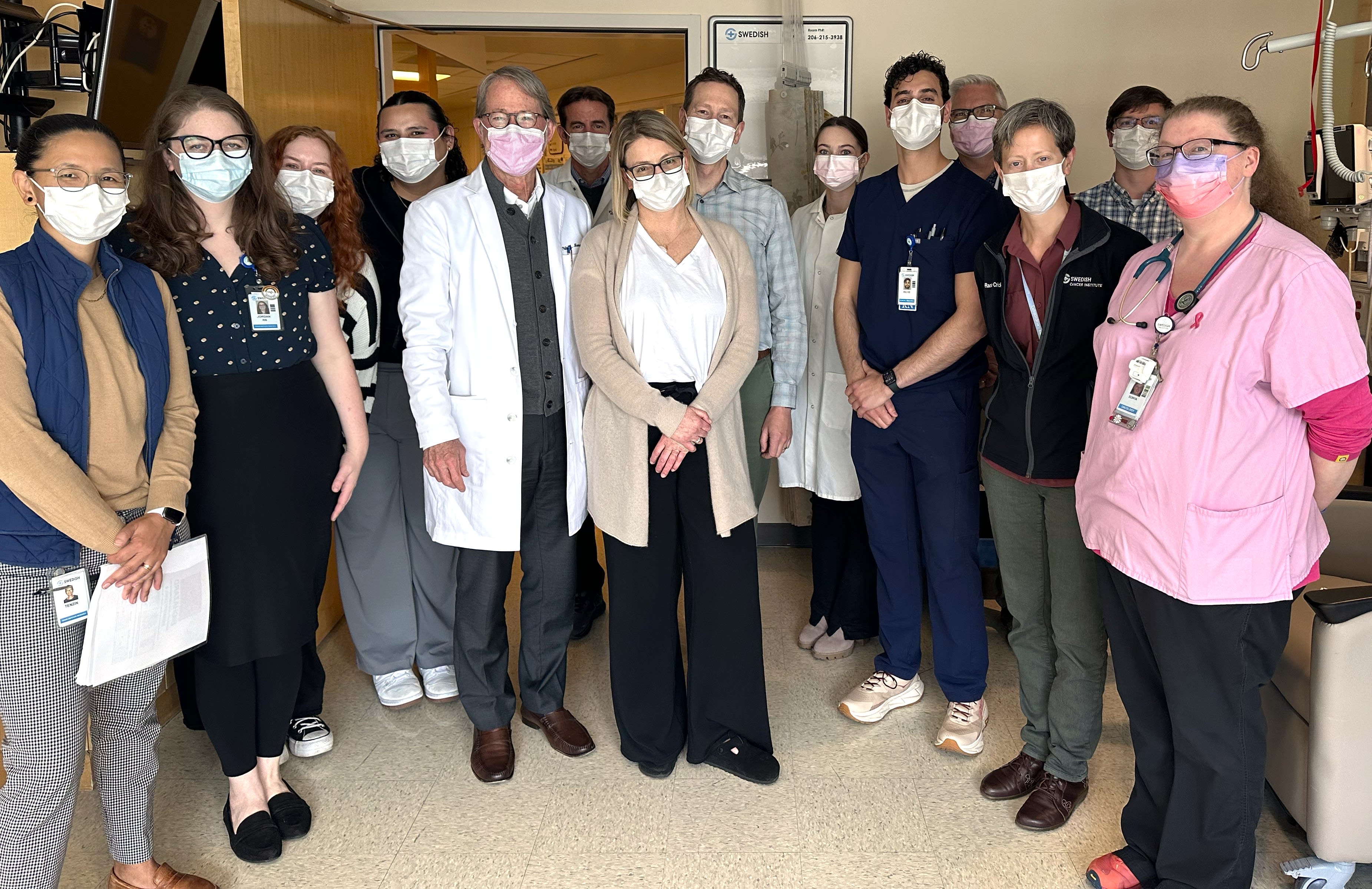
At the Providence Swedish Cancer Institute, we specialize in treating benign blood disorders with a personalized, team-based approach. Our hematology and supportive care experts work together to deliver the most effective, well-rounded care using groundbreaking therapies and the latest treatment innovations.

All blood disorder treatments
Systemic Therapies
- Anticoagulation Therapy
- Blood Factor Replacement
- Immunoglobin
- Iron Replacement
- Monoclonal Antibodies
- Steroids
- Therapeutic Apheresis
- Transfusion
Cellular Therapies
Surgical Therapies
- Interventional Radiology
Additional Therapies
- Antithymocyte Globulin
Advanced Treatments for Benign Blood Disorders
Our personalized approach means we consider specific characteristics of your blood disorder and your health needs to develop your treatment plan. You may receive one or more of the following types of treatment.
Therapeutic apheresis removes or replaces specific blood components — like plasma or cells — to help manage certain clotting issues and autoimmune blood disorders.
Cellular therapies use your own cells to target abnormal ones and restore healthy blood function. They’re often used when standard treatments for benign disorders haven’t worked.
Monoclonal antibodies are lab-made proteins that attach to specific targets on blood cells, treating immune-related or inflammatory blood disorders by blocking harmful activity or marking cells for removal.
What to Expect
At the Providence Swedish Cancer Institute, your care team is with you from diagnosis through treatment, recovery, and survivorship. We combine advanced therapies with personalized care, ensuring you receive leading clinical expertise and the compassionate support you can always rely on, including a trusted, personal relationship with your physician. Learn what to expect during each phase of care.
Evaluation is an important step in helping us guide your treatment with confidence and precision.
We may recommend bone marrow analysis to study blood-forming cells, coagulation diagnostics to assess how your blood clots, and thrombophilia evaluation to identify genetic or acquired conditions that raise your risk for abnormal clotting. These tools help us create a care plan tailored to your needs.
After your evaluation and testing, our specialists work to identify the specific type and cause of your benign blood condition. They’ll review the findings with you in detail and make sure you understand your diagnosis, how it may affect your health, and the treatment options available to support your well-being.
At the Providence Swedish Cancer Institute, your voice is central to your treatment. A personalized treatment plan includes advanced diagnostic insights from your care team, and considers not only the specific type, stage, and molecular characteristics of the cancer, but also the unique qualities that make you who you are — your values, your daily life, and your overall health. Customizing your care can improve outcomes, reduce the risk of recurrence, and support your overall well-being.
We offer holistic care options during and after treatment to support your physical and emotional well-being. Our cancer rehabilitation program is one of only a few cancer rehabilitation programs offered nationally, and it's led by a fellowship-trained cancer rehabilitation specialist. Cancer rehabilitation can include physical and occupational therapy; nutrition management; speech therapy; and lymphedema therapy to address fluid buildup, a side effect of radiation or surgical procedures.
Frequently Asked Questions
You receive care from a dedicated group of specialists working together to provide comprehensive treatment and support. This may include hematologists, pathologists, and infusion specialists.
Our collaborative approach includes nurses, clinical pharmacists, and other experts. Although your care is team-based, you’ll continue to have regular appointments with your lead physician, who stays closely involved and helps coordinate your treatment every step of the way.
Your treatment timeline depends on your diagnosis, overall health, and how you respond to care. Some therapies, like infusions or monoclonal antibody treatments, are given by IV or injection and may be completed in a single visit or over several short sessions — often without the need for a hospital stay.
Cellular therapies typically take place over multiple appointments and may involve a longer recovery period. Your care team will walk you through the timeline and let you know what to expect.
Cellular therapy uses your own cells to help restore healthy blood function or treat disease. We perform autologous therapies, meaning your own stem cells are collected, stored, and then later returned to your body.
Treatment typically begins with apheresis, a process that collects stem cells from your blood. After receiving other therapies, such as chemotherapy, your stem cells are reinfused to help your body recover and rebuild healthy blood cells.
Side effects vary, but your care team will closely monitor your progress, manage any symptoms, and provide supportive care throughout.
We provide a full range of supportive care services to support you during and after your cancer treatment. Some of these services include:
- Art therapists
- Cancer rehabilitation (onco-physiatry)
- Care coordinators
- Genetic counseling (cancer geneticist)
- Health educators
- Medical massage (edema, lymphedema management)
- Music therapist
- Naturopaths
- Nutritionists
- Oncology nurses
- Social workers
- Speech and language pathology
We can also help with finances, food, transportation, and other challenges for eligible patients through our patient assistance fund.
See the full list of supportive care services.
Note: Some services are provided by local partners and vary based on location. Please contact your clinic for more information.
Patients have access to hundreds of clinical trials involving most cancer types. We are often among the first in the U.S. to provide access to Phase 1 trials — the first stage of evaluating treatments in humans. Please note, we open new trials often. Check with your clinician for the latest in upcoming trials.
Learn more and find out if a clinical trial could become part of your treatment plan.
Hair changes depend on the type of treatment you receive. Chemotherapy can cause hair thinning or loss, while treatments like immunotherapy or monoclonal antibodies typically have little to no effect.
Cellular therapies, including stem cell treatments, generally don’t cause hair loss — and in some cases, they may even support hair regrowth and improve hair quality.
If you do experience changes, we’re here to help with support and resources like scalp cooling, wigs, and emotional care to help you feel more like yourself.
Your treatment may impact your fertility, depending on the type of treatment and your individual plan. If you're concerned about fertility, our team will guide you through options, discuss the potential impacts of your specific treatment plan, and connect you with fertility preservation resources to help you make informed decisions about the future.
Our goal is to help you understand the insurance and billing process.
We have financial counselors on staff to help you sort out any insurance issues. These counselors work with your insurance company to verify benefits and coordinate pre-certification or pre-authorization of care if necessary. Then, they coordinate all this information with the medical center’s billing services.
We also have oncology social workers who can help you with:
- Benefits advocacy, if you are eligible
- Financial counseling
- Medicaid applications
- Medicare and coordinating Medigap and prescription plans
News & Info From Our Experts