Autologous Stem Cell Transplant
Restoring Blood Health with Your Own Cells
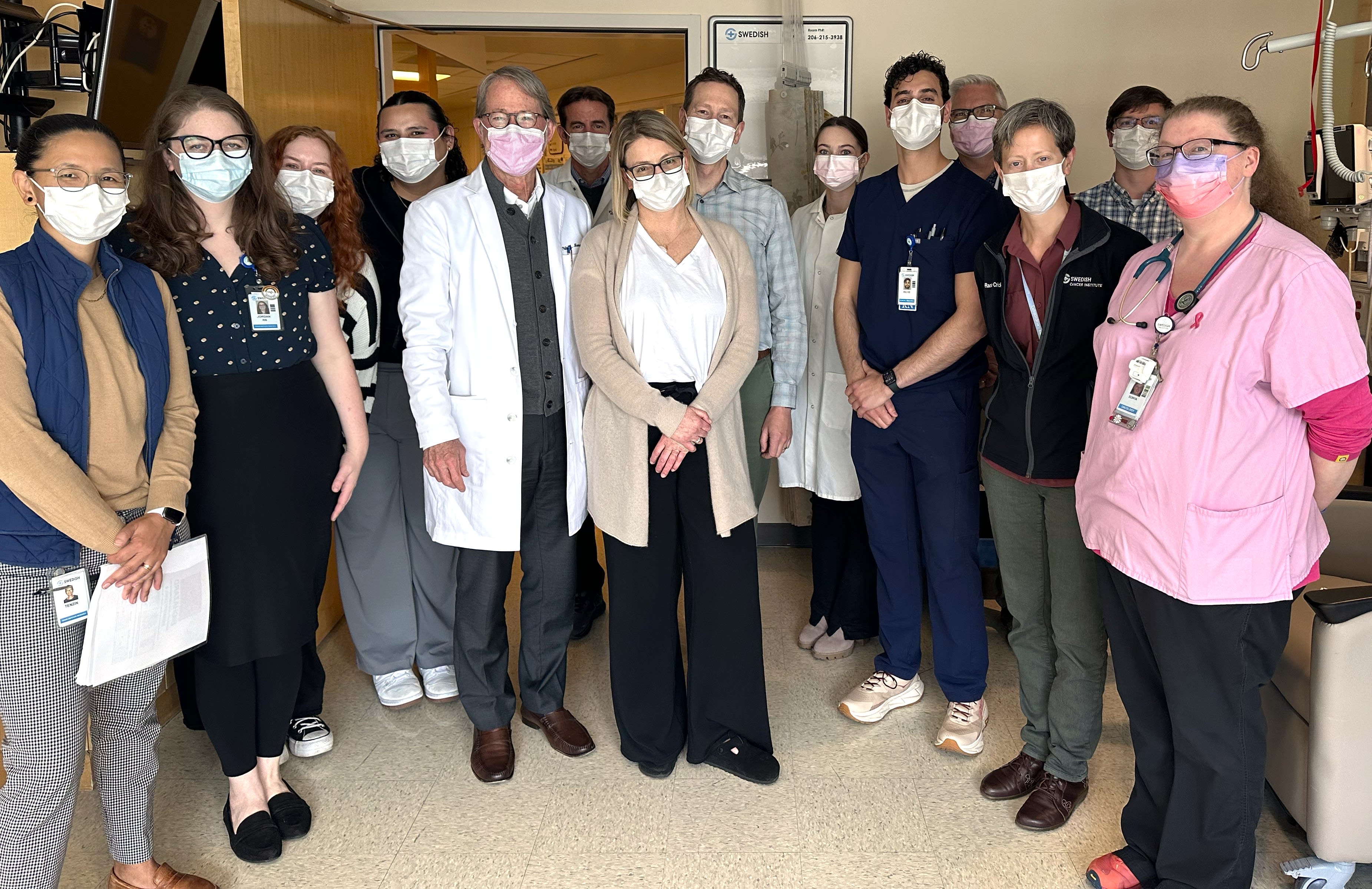
At the Providence Swedish Cancer Institute, our stem cell transplant program offers a life-changing option for patients with blood cancers and other blood disorders. Using your own stem cells, this therapy helps restore healthy blood production and rebuild your immune system. Our advanced techniques support recovery and reduce complications.

Treatment Overview
We use advanced transplant techniques to treat blood cancers and other blood conditions at the Providence Swedish Cancer Institute, always with a personalized approach to your care.
In an autologous stem cell transplant, your stem cells are first collected and preserved. You then receive high-dose chemotherapy or radiation to destroy diseased cells. Afterward, your own stem cells are reinfused to help your body recover and restore healthy blood production.
While the procedure itself is relatively simple, recovery takes time. Our expert team is here to support you — before, during, and long after your transplant.
What to Expect
At the Providence Swedish Cancer Institute, we’ll guide you through the planning stages of your stem cell transplant through to recovery and future treatment if needed. Your care team is here to support your physical healing, emotional well-being, and personal goals, so you can move forward with confidence.
Before your stem cell transplant, we assess your health with blood tests, imaging, and organ function. You may also receive medications or growth factors to help your body produce more stem cells for collection.
Stem cells are collected through a process called apheresis, which separates the parts of your blood using a special machine. Your stem cells are removed, and the rest of your blood is returned to your body. The procedure takes 4-5 hours in an outpatient setting.
After your stem cells are collected and stored, you’ll receive high-dose chemotherapy or radiation over several days to destroy diseased cells. Once your body is ready, the stem cells are reinfused through an IV — similar to a blood transfusion. This begins engraftment, when your body starts rebuilding a healthy blood supply. In the days that follow, you’re monitored closely for side effects and supported with care to manage symptoms and promote healing.
Stem cell transplants can be lifesaving for people with hematologic cancers and some benign blood disorders, helping to restore healthy blood cell production and support long-term recovery. By using your own preserved stem cells, this treatment allows your body to rebuild its immune system after intensive therapy. For many patients, it offers a second chance at remission and an improved quality of life.
As with any intensive treatment, there are potential risks, including:
- Infection
- Low blood counts
- Bleeding
- Fatigue
- Organ complications
Your doctor will talk with you about these risks, answer your questions, and help you manage any side effects that arise.
Your care team is here to support you after your stem cell transplant. You may have some appointments for the first few weeks to help us monitor and manage any complications. Regular checkups are still important so we can continue to manage any of your ongoing treatment needs and watch for signs of recurrence. Services are also available to help you through every treatment stage.
Learn more about our supportive care services.
Frequently Asked Questions
Before collecting your stem cells for an autologous transplant, your doctor runs tests to make sure a transplant is the right option for you. These may include imaging scans (like X-rays, CT or MRI), blood and urine tests, heart and lung checks and bone marrow sampling to see if cancer is in your bone marrow. You also have tests to assess your overall health since high-dose chemotherapy or radiation can put extra strain on your body. If you haven’t had a recent dental check-up, you may need to see a dentist to help reduce the risk of infections during treatment.
You need a dental checkup — including X-rays and a cleaning — before a stem cell transplant to help reduce the risk of infection following your treatment. Because chemotherapy and high-dose radiation treatments weaken your immune system, even minor dental issues like cavities or gum disease can lead to serious infections. Your dentist checks for and addresses any potential problems to help prevent complications during your recovery.
Stem cell collection, or apheresis, is a straightforward procedure similar to donating blood, but it lasts 4 to 5 hours. You can relax with music, TV, or a book as your blood is drawn through your central venous catheter (CVC) and passed through a machine that separates white blood cells, including stem cells. The remaining blood cells are returned to you through your CVC.
You may need to undergo several daily collection procedures before enough stem cells are collected for an autologous transplant. They’re then frozen and stored until they are needed for your transplant.
Some patients experience mild dizziness, numbness, tingling, chills, or lightheadedness during the procedure. If you feel any discomfort, let your transplant or apheresis nurse know right away — they can make adjustments, provide calcium, or offer warm blankets to help you feel more comfortable. Eating a normal meal beforehand and including calcium-rich foods like milk, yogurt, or cheese may also help prevent side effects. Your care team will give you more detailed information and make sure you feel prepared ahead of time.
High-dose therapy may involve chemotherapy, total body irradiation (TBI), or a combination of both, depending on your treatment plan. These intensive treatments destroy cancer cells, suppress your immune system, and prepare your body to receive stem cells.
Treatment is typically given in the hospital over several days. Chemotherapy is administered through an IV along with large volumes of fluid to help manage side effects. TBI is delivered in short sessions that target your entire body. You’ll be closely monitored for side effects such as fatigue and nausea.
A stem cell transplant may sound complicated, but the actual procedure is simple. One to three days after your high-dose therapy is complete, the stored frozen cells are thawed in warm sterile saline and infused through your central venous catheter (CVC). The infusion itself is painless and works much like a blood transfusion. Your care team will closely monitor you for any immediate reactions, such as nausea or chills, and provide supportive care as needed.
After your transplant, the infused stem cells travel to your bone marrow, where they begin growing and producing new blood cells. As your immune system gradually rebuilds over the next few weeks, your care team will closely monitor your progress with regular check-ups and blood tests.
Around 10 to 12 days after your transplant, we expect to see signs of engraftment — when the stem cells start producing blood cells. As this happens, you may feel aching in your bones, especially in your pelvis, lower back, and thighs.
Recovery after a stem cell transplant takes time — sometimes months to a year or more. Fatigue is common. Staying active, even with low-impact exercise like walking, can help you regain energy, but it’s important to pace yourself.
Many patients find comfort in talking to others who have been through a transplant. If you’d like to connect with someone, your care team can help and offer additional resources and supportive care services.
News & Info From Our Experts