Medical Oncology
Targeted Treatment and Personalized Care
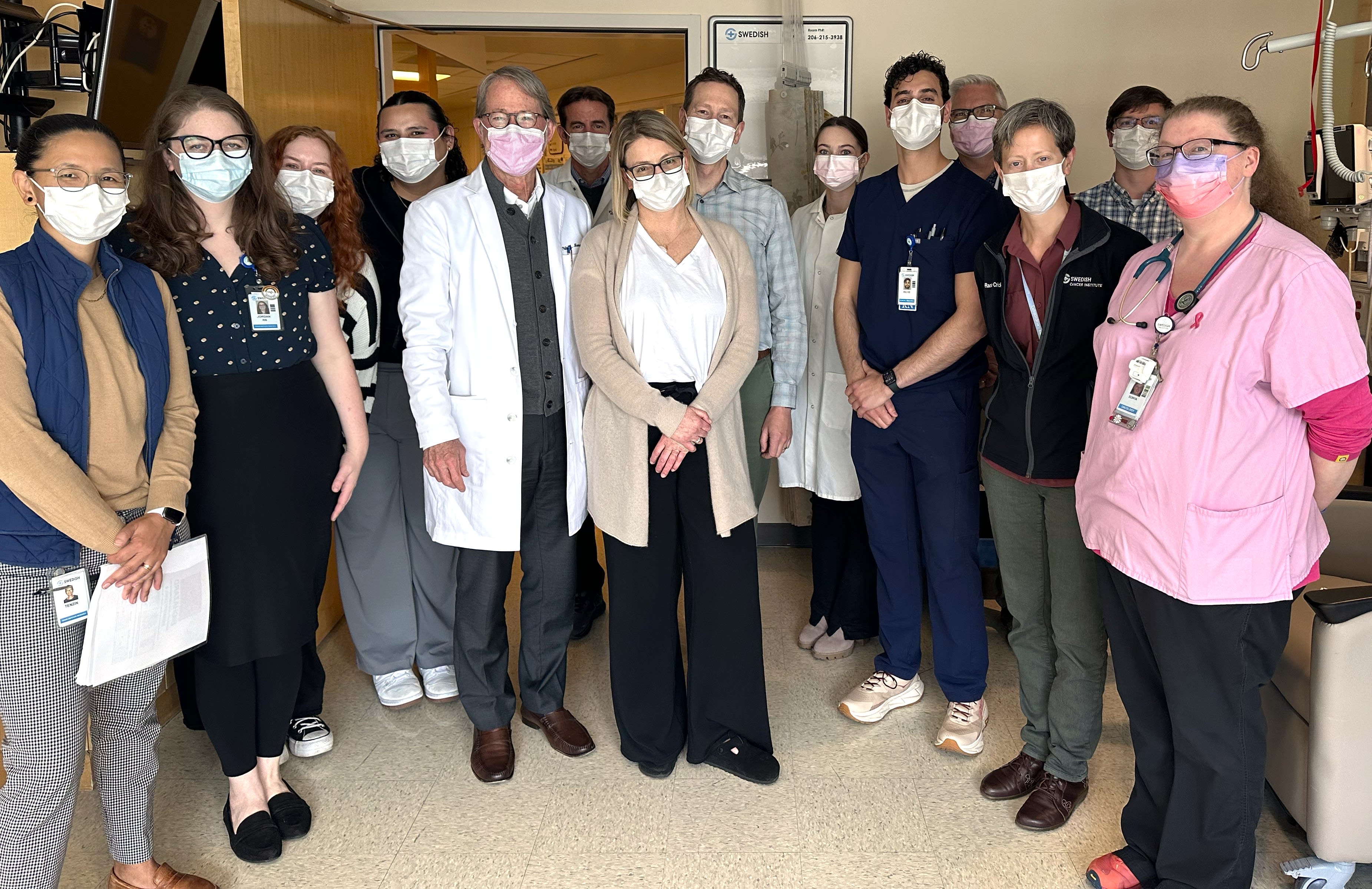
At the Providence Swedish Cancer Institute, your medical oncologist is your dedicated partner from day one. You’ll see the same physician or care team member at each visit. With this level of personalized support, plus access to advanced therapies and cutting-edge clinical trials, you can move through treatment with clarity and confidence.

Where Innovation Meets Individualized Care
At the Providence Swedish Cancer Institute, our expert oncologists bring you the latest in medical oncology treatments–many of which, like CAR T-cell therapy, are not available at most other hospitals in the state.
But it’s not just what we offer — it’s how we deliver it. When you’re in our care, you’ll build a consistent relationship with your physician and a dedicated team that knows you personally. Our focus is on getting you the right treatment, right away, including fast, direct access to clinical trials.
As one of the top clinical trial sites in the western U.S., we offer more opportunities to participate in research than most programs in the region. Our physicians are actively involved in patient-centered trials — those designed to help people living with cancer today, not just years down the line.
Here, leading-edge treatments come with patient-centered care. That means more options and better outcomes.
Advanced Medical Oncology
Our personalized approach means we consider specific characteristics of your cancer and your health needs to develop your treatment plan. You may receive one or more of the following types of medical oncology:
Other medical oncology treatments
Adjuvant chemotherapy is treatment given after your main therapy — often surgery — to help destroy any cancer cells that may still be in the body. The goal is to lower the chance of cancer recurrence. It’s often part of the care for certain blood and solid tumor cancers and can be an important step in giving you the best possible outcome moving forward.
Anti-VEGF therapy represents a family of medications that interfere with the formation of blood vessels in cancerous tumors. Through this interference, they help control tumors by starving them of their blood supply.
Biologic therapies are a type of drug treatment derived from living organisms such as proteins or yeasts. One type of biologic therapy is monoclonal antibodies. These are laboratory-produced agents that target and bind to biologic entities such as receptors on cancer cells.
Biologic therapies use substances made from living organisms to help your body fight cancer or manage side effects from treatment. These may include monoclonal antibodies, cytokines, or vaccines that support or guide your immune system. Biologics are often more targeted than traditional chemotherapy and may come with fewer side effects.
Chemotherapy is the systemic use of cytotoxic chemicals to kill cancer cells. Today there are many medications (e.g., biological medications, immune treatments, targeted therapies) that do not fit the classic definition of chemotherapy yet are often included in this category.
Chemoradiotherapy means you’ll receive chemotherapy and radiation at the same time. Chemotherapy helps make the cancer more responsive to radiation, so the two treatments work better together. For certain cancers, this approach gives you the best chance of shrinking the tumor, relieving symptoms, or preventing the cancer from coming back.
Clinical trials give you access to new treatments that aren’t widely available yet. These studies help researchers find better ways to treat cancer and may offer more options when standard treatments haven’t worked. Your care team will help explore if a trial is right for you.
Cooperative group (NCTN) clinical trials are studies designed by a consortium of leading national cancer researchers. The goal of these studies is to test the newest and most cutting-edge innovations.
Participants in clinical trials may receive treatments not yet available to everyone. They also receive extra follow-up care in addition to their standard care. Taking part in the search for new and better cancer treatments can be personally satisfying, as participants become part of the advancement of medicine.
Every clinical trial has inclusion and exclusion restrictions that a patient must meet before enrolling in the trial. Before you decide to take part, doctors and clinical trial coordinators tell you all the known risks.
What to Expect
Our expert team is here to guide and support you because knowing what to expect can help ease your mind as you start medical oncology treatment. From preparing you for your first appointment to helping you manage potential side effects, we’re dedicated to your care.
Your first visit with a medical oncologist is often the starting point for your cancer care. Depending on how you were referred, this may include an intake visit to review your medical history, past tests, and overall health. Your doctor may order additional tests before making a personalized treatment plan. It’s also a chance to ask questions and begin building a relationship with your care team, which will be led by your medical oncologist.
On the day of your treatment, eat a light meal, wear comfortable clothes, and bring entertainment — such as a book or tablet — to help pass the time. Be sure to let your team know about any medications or allergies in advance. Expect to feel tired after treatment, so plan for someone to drive you home. Most of all, know that it’s okay to ask questions — we’re here to guide you, support you, and make sure you feel ready for what’s ahead.
Treatment plans often span several weeks, with sessions scheduled regularly based on your specific cancer and response to care. Chemotherapy or infusion sessions typically last anywhere from 30 minutes to several hours. You’ll sit in a comfortable chair with blankets, Wi-Fi, and nursing support. Oral treatments are taken at home with regular check-ins. Light activity is usually okay, but it’s important to listen to your body and rest when you need it.
Your care team is here to support you throughout and after your treatments. Regular checkups are important so we can continue to manage any of your ongoing treatment needs and watch for signs of recurrence. Services are also available to help you through every treatment stage.
Learn more about our supportive care services.
Frequently Asked Questions
Medical oncology refers to the use of systemic therapies — medications that work throughout the body — to treat cancer. These include chemotherapy, hormone therapy, immunotherapy, and targeted therapy. Depending on your treatment plan, they may be given through an IV, injection, or pills. Some attack cancer cells directly, while others block growth or help your immune system do the work.
Medical oncology may not be the only part of your cancer care. Some early-stage cancers can be treated with surgery alone. In other cases, surgery may be combined with medical oncology treatments to improve outcomes. Radiation may also be used before or after surgery to shrink tumors or reduce the chance of recurrence. Your care team will tailor the plan to your specific needs.
The number of sessions and how long they last depend on your diagnosis, health, and how your body responds. Some people have treatment weekly, while others have treatment on cycles every few weeks. Sessions can last 30 minutes to several hours, and full treatment often takes several months to complete. Your care team will go over the schedule with you so you know what to expect and can plan with confidence.
Recovery from medical oncology varies for each person. You may feel tired after treatment, and some side effects like nausea, appetite changes, or hair loss can take time to improve. Your care team provides guidance to help manage side effects and support your recovery. It’s important to rest, eat well, and stay hydrated. Many patients return to light activities between sessions but listen to your body and reach out to your team if you need extra care or support.
There’s no one-size-fits-all diet during cancer treatment but eating well can help you feel stronger and support your recovery. Many people find it helpful to focus on small, balanced meals with plenty of protein, fruits, vegetables, and whole grains. A Providence Swedish Cancer Institute nutritionist can help you find foods that work for your needs, manage side effects like nausea or appetite changes, and support your overall well-being throughout treatment.
Some cancer treatments, including certain types of chemotherapy or radiation therapy, can affect fertility. These effects may be temporary, but in some cases, they can be long-lasting or permanent, depending on the type and location of treatment.
If you're concerned about fertility, our team will guide you through options, discuss the potential impacts of your specific treatment plan, and connect you with fertility preservation resources to help you make informed decisions about the future.
We provide a full range of supportive care services to support you during and after your cancer treatment. Some of these services include:
- Art therapists
- Cancer rehabilitation (onco-physiatry)
- Care coordinators
- Genetic counseling (cancer geneticist)
- Health educators
- Medical massage (edema, lymphedema management)
- Music therapist
- Naturopaths
- Nutritionists
- Oncology nurses
- Social workers
- Speech and language pathology
We can also help with finances, food, transportation, and other challenges for eligible patients through our patient assistance fund.
See the full list of supportive care services.
Note: Some services are provided by local partners and vary based on location. Please contact your clinic for more information.
Patients have access to hundreds of clinical trials involving most cancer types. We are often among the first in the U.S. to provide access to Phase 1 trials — the first stage of evaluating treatments in humans. Please note, we open new trials often. Check with your clinician for the latest in upcoming trials.
Learn more and find out if a clinical trial could become part of your treatment plan.
News & Info From Our Experts