High-Risk Screening Program
Personalized Screening for Those at High Risk
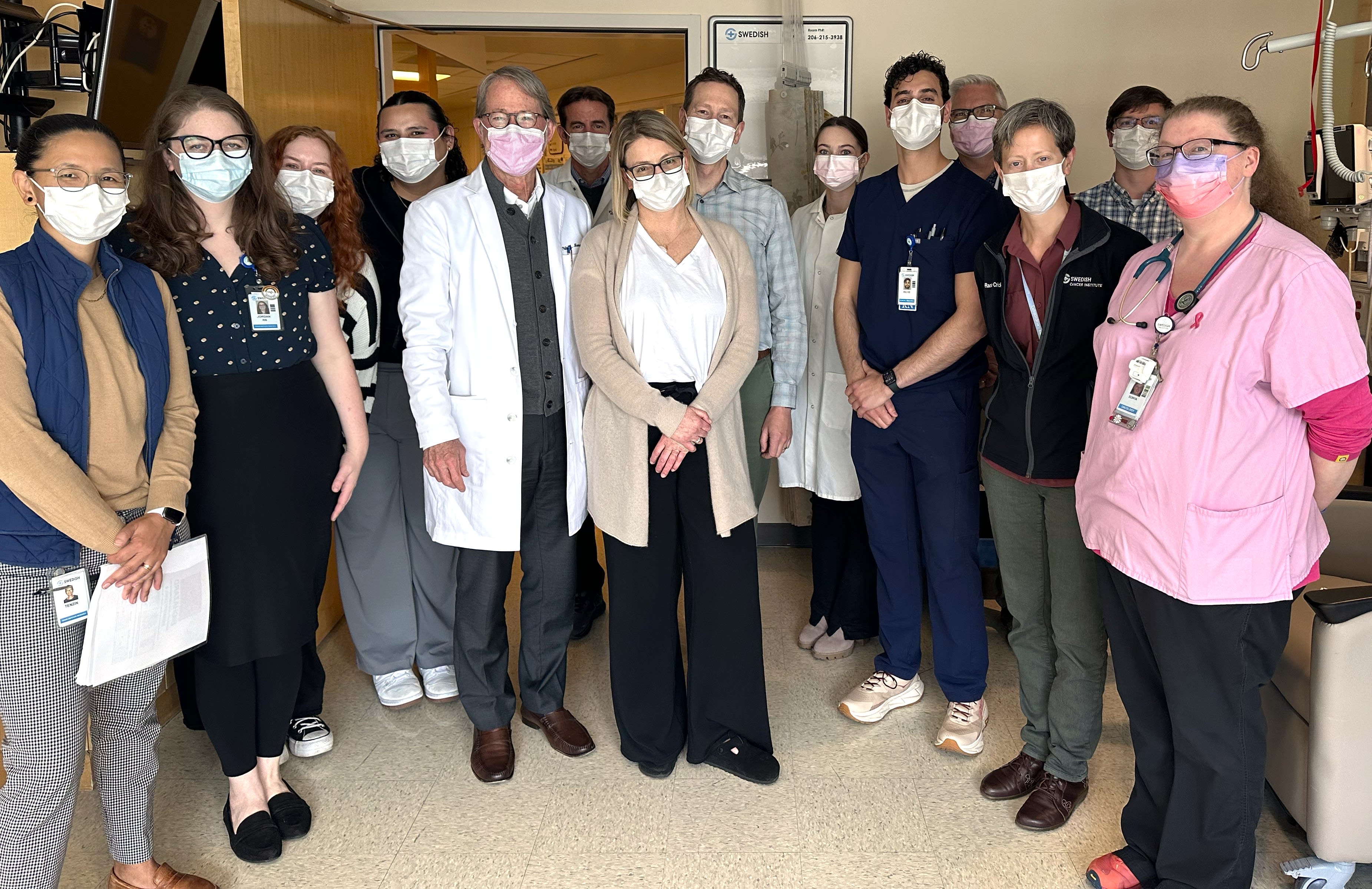
The High-Risk Program at the Providence Swedish Cancer Institute provides comprehensive support to patients identified with a higher risk of developing cancer, particularly breast, prostate, colon or ovarian cancer. We offer personalized education, support, and proactive screening to help detect cancer as early as possible - when it's most treatable.

Our Approach
At the Providence Swedish Cancer Institute, we empower patients with the knowledge and tools to prevent and fight cancer. We believe proactive detection and monitoring are key to managing cancer successfully. We promote and assist with expansive cancer screening programs throughout the institute to give our patients the best chance of catching cancer in its earliest stages – when treatment is most effective.
To determine whether the High-Risk Cancer Program is right for you, our board-certified genetics physician and genetic counselors can help you obtain hereditary genetic tests, an evaluation of your personal and family medical history and review the results of screening tests for specific cancers.
Patients in the High-Risk Program receive a personalized treatment plan from their genetic specialists to help them proactively reduce their risks. This plan often includes one-on-one education and resources, more frequent screenings, recommendations for lifestyle changes, and access to a vast list of specialized support services.
Swedish High Risk Breast & Ovarian Cancer Program
The High-Risk Breast & Ovarian Cancer Program at the Providence Swedish Cancer Institute can address your questions and help you take the next steps in assessing your risk for breast cancer.
What to Expect
As part of the High-Risk Program, expect long-term, comprehensive support from a team that specializes in cancer genetics. You receive a clinical evaluation, risk assessment, and detailed plan to reduce your cancer risk. Our specialty nurse practitioners work one-on-one with you, ensuring you have all the information, training, and resources you need to be proactive about your health.
If you’re interested in the High-Risk Program, we recommend asking your primary care physician for a referral.
Before your initial consultation with our genetic professionals, our staff provides you with a list of materials to bring to your appointment. This includes any of your medical records not on file within the institute system, plus information about your family’s cancer history.
If the results of your clinical evaluation and lab results indicate you are at high risk for developing one or more types of cancer, your genetic specialist will set up a follow-up appointment to discuss your risks.
During this meeting, your genetic counselor answers questions and creates a personalized plan to help you be proactive about reducing your risks. Your plan may include additional testing, preventive medications and supplements, a nutrition plan, and a schedule for regular cancer screenings.
When patients learn they are at high risk, they can make healthy lifestyle changes and begin preventive treatment that may reduce their risk. It also may lead to earlier diagnosis and the identification of targeted therapies. Our nurse practitioners and genetic counselors are also ready to address your concerns and recommend support services for you and your family members.
Frequently Asked Questions
If you suspect that you have a higher risk of developing cancer, we recommend talking to your primary physician first. Your primary care physician reviews your medical records and asks you questions about your family history. They can provide you with a referral for a consultation.
Talk to your doctor about your medical and family history to assess your risk. They can help determine if genetic testing or early screenings are right for you.
Some factors that might make you a candidate include:
- Personal or family history of breast, prostate, uterine, or colon cancer under the age of 50
- Personal or family history of pancreatic, ovarian, or metastatic prostate cancer at any age
- Personal or family history of breast cancer in both breasts
- Multiple people in the family with the same kind of cancer
- Personal or family history of over 10 pre-cancerous colon polyps (adenomas) or rare tumors like pheochromocytoma, paragangliomas, male breast cancer or adrenocortical carcinoma
We recommend checking with your insurance provider to see if they cover genetic testing and any services or treatments your genetic counselor prescribes as part of the High-Risk Program. Most insurances, including Medicare, cover genetic testing, but not all cover your initial consultation with a genetic counselor. Most insurance will cover your visit with a physician after your genetic results are back.
During your initial consultation, your genetics counselor asks multiple questions about your personal and family medical history. Gather as much information as you can, including your medical records, your and family members’ previous genetic testing results, and a list of family members who have or have had cancer. Include details about their diagnoses, such as age, cancer type, and outcomes.
Your genetics counselor uses this information to evaluate whether you need testing and which tests to order as needed.
If you were adopted or have little information about your biological family, it is okay, your genetic counselor can still help you get the test.
If you’re identified as being at high risk for cancer, it doesn’t mean you will definitely develop cancer. It means you have a greater likelihood of developing cancer compared to the general population due to genetic mutations, family history, or other risk factors. However, lifestyle and environmental factors and random chance also play a role.
Your care team can discuss these factors with you and help you develop a personalized risk reduction plan, which may include more frequent screening, lifestyle modifications, or preventive measures to lower your risk and support early detection.
In our High-Risk Program, you typically have two clinical exams each year — one with your primary care provider or gynecologist and another as part of the program’s specialized screening. We also recommend annual mammograms for all patients, regardless of risk level, to support early detection and peace of mind.
Being high risk for cancer doesn’t directly impact fertility, but some risk factors – such as genetic mutations like BRCA1 or BRCA2 – may factor into your reproductive health. Additionally, if preventive treatments like surgery or medication are recommended, they could affect fertility. Our fertility experts can meet with you to discuss options for fertility preservation and for embryo testing.
If your screening results show something abnormal or unexpected, we know it feels concerning — but it doesn’t necessarily mean cancer. Your doctor may recommend additional tests, like imaging, bloodwork, or a biopsy, to get more clarity. No matter the outcome, your care team is here to support you, answer your questions, and guide you through the next steps.
News & Info From Our Experts